Pediatric Liver Transplant
What is a Pediatric Liver Transplant?
A Pediatric Liver transplant is a surgical procedure that is done to treat Liver failure. The liver is essential for digesting food and removing all the toxic substances from your body. If your Childs’s Liver stop working, then the liver will not be able to filter harmful substances from their blood and it can lead to Liver failure which is a life-threatening condition.
A liver transplant is a surgery to replace a diseased liver with a healthy liver from an organ donor. The new liver may come from an organ donor who has just died, or part of a liver may come from a healthy living person which is called a living donor. A living donor can be a family member, or someone who is not related to your child but has a matching blood type.
People who donate part of their liver will have healthy lives with the liver that is left. The liver is the only organ in the body that can regenerate the damaged tissue, which means that the donor’s liver will grow back to normal size after surgery. The part that your child receives as a new liver will also grow to normal size within a few weeks.
What are the Functions of the Liver?
The functions of the Liver are as follows:
- removing toxins from your blood
- converting nutrients from the foods you eat
- storing minerals and vitamins
- regulating blood clotting
- producing cholesterol, proteins, enzymes, and bile
- making factors that fight infection
- removing bacteria from your blood
- processing substances that could harm your body
- maintaining hormone balances
- regulating blood sugar levels
Once the Liver is damaged it loses the ability to perform the above functions.
Want more clarification about medical expense & treatment plan?
Plan Your Pediatric Liver Transplant In India
Why might my Child need a Liver Transplant?
A liver transplant is recommended for children who have serious liver problems and could die without a new liver. The most common liver disease in children who will need transplants is biliary atresia. This is a rare disease of the liver and bile ducts that occurs in newborns.
The other conditions may include:
- Liver cancer and other liver tumors
- Sudden or acute liver failure due to an autoimmune disease, unknown causes, or an overdose of medicine
- Other genetic and hereditary liver diseases
- Conditions present at birth, namely Alagille syndrome or cholestatic disorders
- Viral hepatitis
- A build-up of too much iron in the body, which can damage organs.
What are the Types of Pediatric Liver Transplant?
There are two ways that your child can get a donated Liver:
Deceased donor: Your child may get a Liver from a healthy person who just died. To get a deceased donor transplant, the name of the child must be added to the national waiting list for an organ. The wait for a Liver could take many months or years.
Living donor: A healthy, living person may donate one of their Liver to your child. After donating their kidney, the donor will continue to live a normal and healthy life. Almost a half of Liver transplants for children, are from living donors.
The surgery will be planned in advance if the liver is from a living donor. Both, your child and the donor will have surgery at the same time. Donors for children are often their parents, siblings, or other family members. Parents of a child are the best donors because they often have the same blood type.
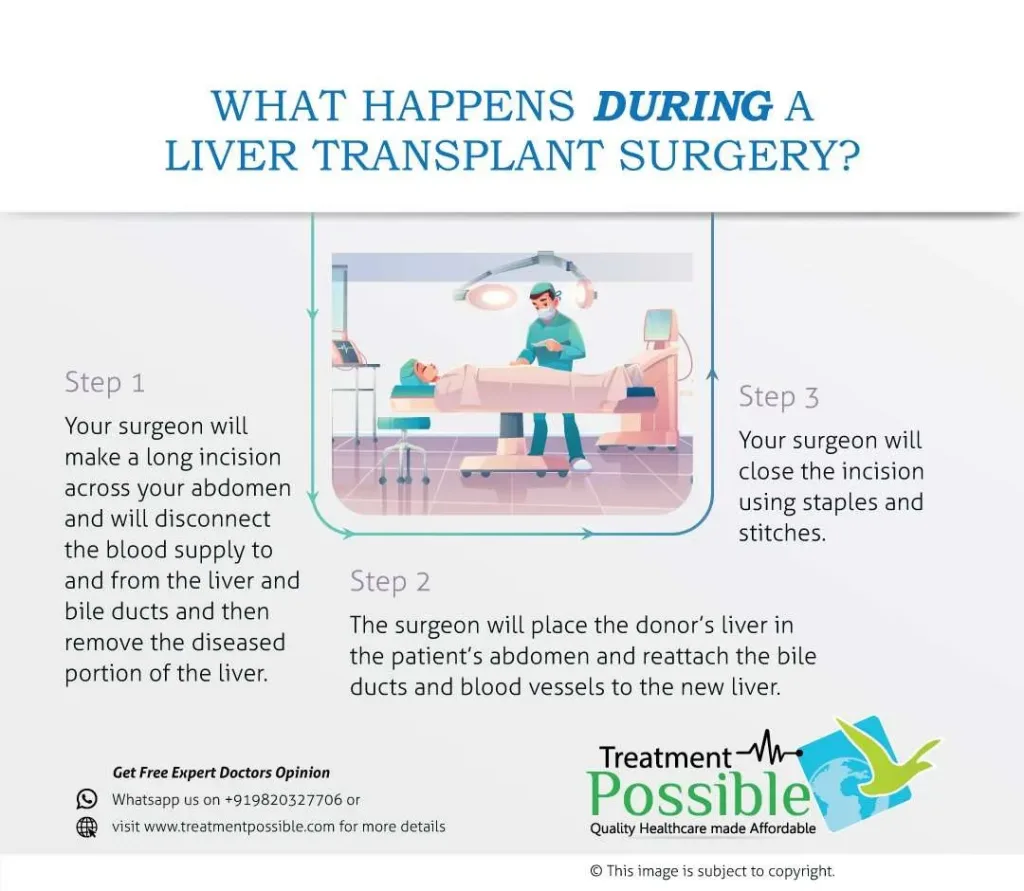
What happens during the Pediatric Liver Transplant?
Your child’s surgery may take four to 12 hours depending on his or her condition.
- Step 1 – Your child will be given general anesthesia so that he or she is in a deep sleep. After your child is sedated, the anesthesiologist will put a tube into your child’s lungs. This is done so that your child’s breathing can be helped with a ventilator. The anesthesiologist will keep checking your child’s heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- Step 2 – The surgeon will make a cut or incision just under the ribs on both sides of your child’s belly.
- Step 3 – The surgeon will carefully separate the diseased liver from the nearby organs and structures. The arteries and veins will be blocked so that blood does not flow into the diseased liver. Then the diseased liver is removed after it has been cut off from the blood vessels.
- Step 4 – The surgeon will check the donor liver before implanting it in your child’s body. The donor liver will be attached to your child’s bile ducts and blood vessels then the blood flow to the new liver will be started. The surgeon will check for any bleeding in the stitches. The surgeon closes the incision with stitches or surgical staples. A drain will be placed in the incision site to reduce swelling.
Living after a Liver Transplant:
Rejection is a normal reaction of the body’s immune system to a foreign object or tissue. When a new liver is placed in your child’s body, the immune system attacks it thinking it is a threat. To help the new liver survive in your child’s body, your child must take anti-rejection medicines, also known as immunosuppressants.
Immediately after surgery, the dosages will be high since the probability of rejection is the greatest at that time. Dosages will be lowered quickly to smaller amounts if there are no signs of rejection. The medications will have side effects in the beginning when the medication dosages are high. As the dosage is lowered, these effects will probably be reduced. These medicines weaken the immune system’s response. Your child must take these medicines for the rest of their life.
Living with a liver transplant is for a lifetime. Your child has to take anti-rejection medicines so that the immune system won’t attack the new liver. Other medicines should be given to prevent side effects of the anti-rejection medicines and these side effects include infections. It is important for you and your child to keep in close contact with the transplant team.
